On May 12th, I went to my new physical therapy office. I had decided to keep the referral even though the injections hadn’t done anything for my chronic pain.
My new physical therapist is a quiet woman with an Eastern European accent who calls everyone sweetheart. Very different from anyone I’ve had before. She’s also a little blunt, which is a little funny. She said she’s worked with several people with CP almost exactly like mine and they all improved. “You need to stretch. You need to get stronger.” To the student PT, “Look, she has no range of motion. This is neutral and it’s tight.” On and on. Explaining me to myself. I mean, I know there’s a possibility of improvement, and I know there comes a point when there’s not. At least she demonstrated a sound grasp of my mechanics.
What I really liked was at the end. They’re very into modalities at this place. I got to have e-stim (TENS unit) put on my low back and right glute, with a giant ice pack over the whole area, a pillow between my knees, lights off and the door closed, and a little bell right next to me in case I needed anything. I assumed I was in a room rather than out in the main area (here they didn’t even have curtains between the tables) because I was a new patient, and I was grateful. I don’t think it helped at all, but it was nice just the same.
The therapist had given me similar if not identical exercises and stretches as everyone else, no surprise there. She tried to give me ones that I could do on the bed, so I wouldn’t have to get up and down from the floor, which I appreciated. Then it’s that whole, “Do these several times throughout the day. It’s just a part of your life now.” Or break up one set of ten throughout the day until you’re stronger. I have absolutely no reason not to incorporate these things into my life, and yet I don’t successfully do it. Still, I do try some days. Against my better judgment, a day or two after that appointment, I got on my hands and knees on my bed and tried to lift a leg out behind me. I knew this was too hard, even though I had done it on the table under the PT’s supervision. I knew the bed wasn’t an appropriate surface to do something that was on the edge of my ability. Even though I tried to keep my core tight, my back bowed and protested sharply. And as seems to be the way with my body these days, I acquired an additional back injury that hasn’t healed a month later. It’s really made functioning so much more painful and disheartening. So there’s that.
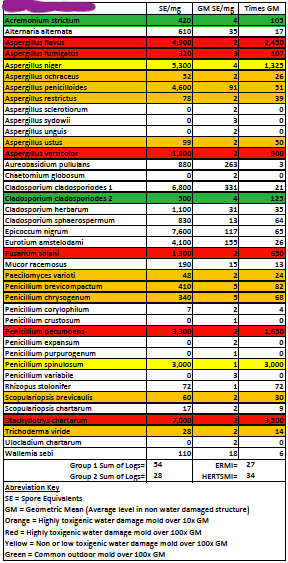
Immediately following that first PT appointment, I had the allergist appointment. I brought a typed list of my throat history and all the mold testing data. I explained that I was looking for some confirmation of mold issues before we tore our house apart. I knew there wasn’t “a mold test.” I brought up my tTG numbers and the possibility of additional autoimmune diseases. I had even found one that fit so many of my symptoms–including a sore throat. He chuckled (nicely) and said no, I don’t have that. “People with that are really sick.” But he ordered the test for it anyway. I don’t have it. He also ordered a test to see if I’m allergic to mold. It was a standard allergy panel that included five common molds from my local area (none of which were the molds in my house). I am not allergic to cat dander or pollen or any of the dozen things on that panel. But he can do skin tests anyway, if I want. I do not. He said I should get the mold in my house cleaned up anyway, because mold isn’t good for people.
At my second PT appointment two weeks later, I told her about my back and we modified some things. Then she told her student/assistant to get the cupping ready. I wasn’t super excited about that, because I’d had it done a couple times when I had acupuncture and I do not enjoy it. However, they did a very mild version, where they lubricate the cup and move it over the skin–no leaving it there to create baseball-sized marks. I also got to have the e-stim and ice pack in a dark room again. Three modalities in one appointment–ooo, nice. Did they help with the pain? No. Whatever else we did, I think I felt a little looser at the front of my hips, which is always nice and doesn’t last long, no matter how much I try to maintain it.
June 9th, I finally, finally had the appointment with my new primary care doctor–the appointment I made back in March just so I could get into the UC Davis system for my sports medicine referral. I was looking forward to a new doctor, new perspective, someone who might look over everything again and put the pieces together in a new way. Plus, she’s certified in family medicine and psychiatry, and I’m really appreciative of that combo. I was hoping I’d get a referral to rheumatology out of it.
My new doctor had a resident with her, who took over all the typing/computer stuff, so my doctor was actually looking at me and listening to me rather than typing, and I really like that. I had typed up (on a single sheet) my top five issues and their symptoms, plus additional symptoms that may or may not shed light on anything. Yes, I’m someone with five major things, and yet I am not a hypochondriac. I put cerebral palsy as one, “mold issues” as another, etc. The thing about being a patient, though, and not a doctor, is that I don’t know for certain what the relevant information is for each column, or what I’m leaving out.
After talking to me and looking over the sheet, the doctor asked what I wanted to focus on, and I said my sore throat and burning forearms, because those are the ones that don’t make sense. Because my forearms burn and at the beginning I had lost grip strength and I have constant neck pain, she thinks it may be a nerve issue. Get this, she recommends I get the nerve conduction study/EMG on both arms! Ack. And they proceeded to try to add it to the one for my legs coming up at the end of the month. Let’s just torture all the limbs, shall we? I was a little stunned that she already recommended this kind of procedure. (In my mind, I’m connecting it to mold because it started literally when we began sheltering in place. But obviously, if you don’t go with mold, there’s a different cause.) And I realized, after the initial appointment for my arms with my prior primary care doctor, and the PT that helped with grip strength but didn’t stop the burning, I haven’t followed up. So maybe I have a pinched nerve in my neck.
We discussed my chronic pain(s), and everything I’ve tried that hasn’t worked. She said, “I can think of five medications right now that might help you. So let’s start with the one that has the potential to do the most good for the most issues.” So now I’m taking gabapentin. I was offered this once before, years ago, and decided not to take it. This doctor talked me through it though: “We start you on the lowest dose and if you tolerate it well, gradually increase it. If you have side effects, you’ll stop taking it and the side effects will stop. It’s a relatively low-risk thing to try.” Sounds reasonable. Ironically, the most common side effects are tiredness and feeling unstable/dizzy. Great, because it’s not as if I’m not already exhausted and unstable.
We also talked about my throat, all the treatment I’ve been through, the tTG numbers. They looked at the pictures I brought of my upper endoscopy. I conveyed my frustration over the two ENTs treating me for two very common conditions (reflux and general inflammation) and then throwing up their hands. She wants to send me to gastroenterology. I only saw a GI doctor for the endoscopy and the follow up on video. So being sent to a GI sounds fine. But I was disappointed that she didn’t feel rheumatology was warranted.
She did notice that I put positive ANA under the autoimmune column on my sheet and asked what other tests that integrative medicine doctor had ordered. I didn’t remember, but directed them to June 2018 when I had loads of testing and was diagnosed with celiac.
I have looked over these tests many times over the years, and googled each flagged result. I remember mentioning CREST to the GI doctor when we were about to do the upper endoscopy in October 2020. “CREST? You have CREST? You should see a rheumatologist,” he said. “Oh,” I said. “Well, I have Raynaud’s.” I didn’t know if I really had CREST, but I remembered that the R was for Raynaud’s and that I have that (we assume).
My new doctor and her resident scrolled through my labs from 2018 and talked to each other, and I heard my doctor say, “Oh! You can go to rheumatology.” That integrative medicine doctor had ordered the tests in 2018 that my new doctor would have ordered before confirming the need for a rheumatologist. “You have a high centromere antibody. Has anyone talked to you about that?”
The answer is no. When I got home, I read back through the notes on the test results from the integrative doctor in 2018. I was a new patient, so she’d ordered a full work up, and there were lots of results to go through. She never said anything about that one. I probably figured since I had the R in CREST and that Raynaud’s is not a big deal, that there wasn’t anything that needed to be done, and I never asked anyone about it directly. Though clearly I’d looked it up at some point, and told the GI doctor I had CREST. Here’s what it says right on the test result from Sutter Hospital:
Centromere antibody is virtually diagnostic for the scleroderma variant known
as CREST (calcinosis, Raynaud’s phenomenon, esophageal dysmotility,
sclerodactyly, and telangiectasia).
This doctor asked if I had any skin concerns and studied my hands. No doctor has ever inspected my hands that way before. Ooh, she’s good, I thought. Really examining the patient and looking for signs, rather than just sitting at the computer. After I came home and looked up CREST again, I realized she was looking for symptoms of sclerosis. Notice that the E in CREST has to do with the esophagus. So far, I haven’t had difficulty swallowing, and nothing mentions chronic sore throat, so we’ll see if there’s anything there. Also, apparently now it’s “formerly CREST” and is officially called “limited systemic sclerosis.” It’s rare and doesn’t sound great because it can mess with your organs and all, so…
Since seeing that integrative medicine doctor in 2018, I’ve seen my PCP, two ENTs, a GI doctor, a functional medicine MD, and an allergist. Seven doctors. It seems as though the original doctor who ordered the test dropped the ball, and no one picked it up. I don’t know if or how things would have been different if I’d gotten a rheumatologist referral four years ago. No use in thinking about that.
As I was writing this, I received a notification that my rheumatologist referral had been processed and I could call and make an appointment. So I did. There’s one available tomorrow at 11am. Or in September. So I took the one for tomorrow.
Now it’s tomorrow, and it’s 10pm. We left the house at 10:15am to arrive at 10:45 for our 11am appointment. I filled out the pages of new-patient forms (they were not looked at). My doctor didn’t arrive until almost noon. He gave me an elbow bump and apologized multiple times for the wait. He was with us for about an hour and it felt very thorough. Went through all the symptoms and pains, even ones that don’t seem related to each other. (This rheumatologist is also an orthopedic surgeon!)
We talked a lot about my burning forearms and burning toes. He looked at my toes. He looked at my capillary nail folds on my hands. A dot of clear soap at the base of each nail, a light, and a little magnifying glass. Fun. This was to check for sclerosis. He looked at my scalp and at my throat. He looked through my previous labs.
He came to a few conclusions: He doesn’t think I have Raynaud’s because there’s no color change. The burning toes and the forearms seem like neuropathy. Even with the positive ANA and the centromere antibody thing, I have no signs of systemic sclerosis. Well, I have two mild ones, but no skin changes. At this time, he sees no active autoimmune disease. I do have a possibility of developing lupus or sclerosis, so I will see him every six months for a bit. He doesn’t know why I have a sore throat. And he doesn’t know why my tTG has gone way back up. He even said something like, “Well, this probably wasn’t a very satisfying visit. But it’s good to know you don’t have another autoimmune disease.”
So there we are. He ordered a few labs, mostly because I’m new and don’t have any labs in UCD’s system. And he referred me to a neurologist. That’s right, I got another referral. Maybe the next one will be able to help me.
I did my labs in the same building. I had to do a urinalysis, and I have to say–I did my best one yet. It’s difficult to do a clean catch when you’ve got to hold yourself up in a kinda squat with one hand and manage the cup properly with the other. I didn’t even get any pee on the outside of the cup! Go me.
I’m not super hopeful about the new referral. But I’ve never been to a neurologist (well, at least not that I remember), so it should be an interesting experience.
It does feel like referral after referral, getting passed around, no one knowing how to help me. Such is life with chronic issues. I’ll keep trying to calm my central nervous system and try not to think about the EMG coming up at the end of the month.