I’m still here, still struggling both mentally and physically. I haven’t felt like there’s anything much I want to say. But Disability Pride Month has come around again, so here’s a link to last year’s post which still sums up things for me nicely.
I have been feeding my YouTube addiction with some new content. I already follow several people with disabilities, and YouTube recently suggested a new one to me. Brooke Eby (@limpbroozkit) who is mainly on Instagram and TikTok, I think, as her content is usually short form. She started making videos 3 years ago when she was diagnosed with ALS. I was sucked into her story because she’s a fast talker with deadpan humor and great hair. Brooke was 29 when she started having symptoms and 33 when she was diagnosed. It started with weakness in her left leg, which is also my weakest limb. She has a video that shows the progression of her symptoms and mobility aids. She starts by wearing a small brace on the left foot, then a bigger brace and a cane, then braces on both legs, a walker, a wheelchair. In later videos, she displays her stiffening fingers, how she can no longer lift her arms, and how she discovered that with a weak core, it’s difficult to cough and blow your nose.
ALS can start in a limb, like it did with Brooke, or it can start in the throat and affect your ability to speak and eat from the beginning. Every three months Brooke goes to the hospital for her breathing test and every three months she gets to know how much worse she’s doing. When she started, her lung capacity was over 100 (out of 100), and now it’s in the 30s. Or it was when she last made a video about it. She wears her bipap (a noninvasive ventilation device) almost all the time now. And she recently got a feeding tube because even though she doesn’t need it yet, she needed to do the surgery while her breathing was still strong enough that it was safe to be under anesthesia.
It’s been a decade since the ALS Ice Bucket Challenge, which dramatically increased awareness of ALS and raised a lot of money for research, but has not yet led to effective treatment. The average lifespan after diagnosis is two to five years. We think of ALS as a rare disease, but it is not. It occurs in 1 in 300 people. It’s just that it kills people so quickly that there aren’t many people with ALS alive at one time.
YouTube doesn’t feed me these short videos in chronological order, and it’s so disconcerting to see a more recent one and then watch an older one in which the disease hasn’t progressed as far. First, she’s showing us tools that she uses to make her solo apartment in New York more accessible, and then she makes a video about moving back in with her parents. From watching Brooke and her dad demonstrate how they use a lift, to going back in time to Brooke putting accessible shoes on, doing her makeup and brushing her hair. It’s wild to have this video record of the speed at which ALS changes someone. Brooke says that hers is a slower-progressing form and that it’s slow enough for her to make the mental adjustments and get used to it. For me, it’s hard to watch someone show off their new electric can opener in a video from a couple years ago, and know that now she cannot grip the can opener at all. It seems that as fast as she and her family acquire the right equipment to help them live, her needs change again. One in 300.
So why am I obsessing over Brooke’s story, checking for updates, wondering how much longer she’ll be able to use her voice? ALS reminds me so much of CP. Only it’s like the person with ALS is going through CP in ALL its forms, on fast forward: the muscle weakness and stiffness, lack of control, the various mobility aids, the need to constantly adapt. But CP doesn’t kill you and ALS does. Why haven’t we figured out an effective, accessible treatment yet?
There’s a quote, apparently by Theodore Roosevelt that proclaims, “Comparison is the thief of joy.” If we compare ourselves to other people who seem to have it better than we do, we feel sad, frustrated, jealous, inadequate, etc. But often, in the context of disability content, we’ll see lots of comments like, “I thought I had it bad, but after seeing what you’re going through, my life is looking pretty good!” It’s insensitive and insulting. Basically, “Wow, sucks to be you!” A terminal disease, while disabling, is very different from other physical disabilities. ALS does suck. We actually do need a cure for ALS. Am I seeing my cerebral palsy from a different perspective after following Brooke’s journey? Yes. I think people with CP are good at not taking the abilities they do have for granted. I have always been so very aware of, and so very grateful for, my ability to use my hands and fingers, to speak clearly, to use the bathroom alone, to roll over in bed even though it isn’t easy. But after learning more about ALS, I have also been savoring my ability to take a deep breath, to swallow, to scratch my nose. It’s a different feeling, a more accepting one. Yes, my body hurts. My throat pain is a constant because the muscles are tight. It’s true that my body can no longer do what it once did and that it will continue to decline. That is not unique to me, or to cerebral palsy. So many people are living with unpredictable, undependable, painful bodies. For so many reasons and in so many ways. I am in good company. It feels better, to not be struggling alone, but to be one of many who are living on the “my body is not typical” spectrum. When I stand up from a chair and my feet and back are so stiff and painful that I can barely straighten up and move, I try to remember that that is just fine. That is how things are, and it’s okay for my feet and back to be stiff, to hurt. It’s part of being me, of being alive. It’s as if all those years of meditation practice, about acceptance and surrender, might just be starting to mean something to me.
People with disabilities are the largest minority and the only minority that anyone can join at any time. That may sound ominous or threatening, but it is only the truth. After I watched Brooke’s videos, YouTube’s algorithm suggested other people with ALS to me. One is a 21-year-old girl, whose whole body is affected already, and who, if I didn’t know her diagnosis, I would think had CP. But she is dying, both slowly, and much too quickly. YouTube continued to suggest other people with disabilities, too, paraplegics and quadriplegics. A skiing accident, a car accident, even a hammock accident (which is more common than you think), and people’s lives become so different than they could have imagined or planned for. Every spinal cord injury is unique; there’s so much variation in how much sensation and movement is recovered. Some people are still very independent with their activities of daily living (ADL) and some people need almost complete care. And some of those people choose to share their lives online and show us what it’s like to use a catheter to pee, have a “bowel program” to poop, or have a preferred person feed them because that person takes the time to create a well-balanced bite. From an able-bodied (and probably uninformed) perspective, it’s all about walking again, but there’s so much more to life and to living than walking.
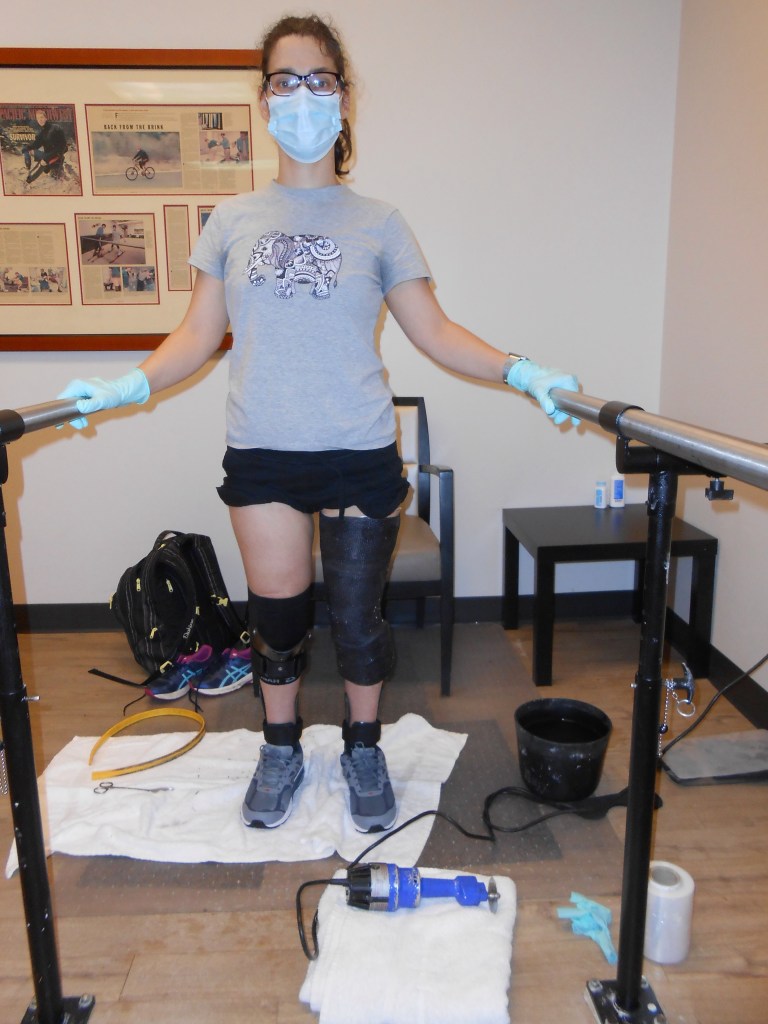
So many people with illnesses, injuries, and disabilities don’t have the option of choosing braces today or not, walking poles today, or walker. They use the tools they need to use to live, whatever those tools are. I’m still at a place in my life and my disability where I have a choice in some ways. The choice to walk out the door without a mobility aid is gone, but options still abound in other ways. And that’s simply how life is. All these statements I’m making are not revelatory. I’ve thought these thoughts before. They’re just making a softer landing in my mind these days, and settling in.