I’d love to be able to write that since October, there’s been much progress and improvement on fronts cerebral palsy– and mold-related. But I am not able to write such things.
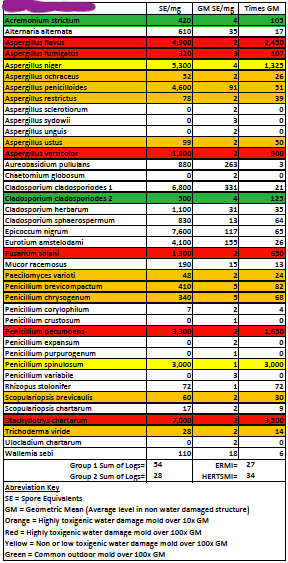
With the mold, we had been waiting, waiting for results and estimates. We got the mold culture back later in October. The culture was taken from the original dust sample, and then it took a while to see what was still active and growing in that sample. Out of all the scary oranges and reds on our ERMI (see previous post), there were only five active molds in the culture. And the alarming “black mold” was not one of them. So we don’t have any active black mold, but there’s still lots of old black mold spores that need to be cleaned out of our house. At least, that’s what I gathered from the whole thing.
After the culture, we then had “Pathways” testing done. Rather than have someone come and start pulling up baseboards and just look for the mold, we had the whole interior perimeter of our house sampled (and around windows) to see where the mold might be coming from in a nondestructive way. We found, unsurprisingly, that there’s a strong indication for mold under our sink/dishwasher, and around our skylight, as well as a couple other odd places. (Even though we’ve not seen water damage it doesn’t mean it isn’t there.) But since then in early December, we’ve made no progress. We are still waiting for the remediation company to give us an estimate based on the Pathways results. Should be any day now.
We have been advised that our original 1980s skylight will need to be replaced once remediation is complete. Did you know that no one makes ten-foot skylights anymore? No? Neither did we. We have one long, narrow skylight above our front door. Lots of light. Lots of trouble. We are going to have to put in two or three smaller ones, in place of the big one. That just means more potential for leaking skylights in the future, though. Skylights are notorious for leading to water damage. One smaller one, and close up the extra space? We could close it up altogether, but we do like the light. I do not enjoy this part of adulting/home ownership.
I do very much want to get the mold dealt with so that I can see if I will indeed start feeling less sick. I’m so tired all the time. Exhausted by the throat pain, like I have strep throat every day of my life, tired of my forearms and my hands hurting. These aren’t CP things, so I need them to be mold things. I want CIRS to be what’s happening, because that means I have a chance of someday feeling better than this.
On the cerebral palsy front, I had been waiting on a referral to UC Davis to see a pediatric orthopedic surgeon who is familiar with both (younger) patients with cerebral palsy, and open surgery techniques in case that is what my hip was going to need. Eventually, I received a letter from UC Davis turning down my referral. I’ve never been given a flat-out no like that. They said they just don’t have the time/doctors. I let my doctor know, and they said they’d keep looking for other options for me. But, I didn’t hear anything.
I recalled that from my own research, there are two places I know of in the United States that specifically state that they work with adults with CP: the Weinberg Cerebral Palsy Center in New York and the Center for Cerebral Palsy at UCLA. They hold two clinics weekly and one of them is a “lifespan clinic,” meaning that they see adults.
It sounded very fancy and hard to get into. I filled out the online form and was never contacted. So I had my doctor send a referral and was never contacted. Then I called the number and it was the general UCLA Health number (“If this is a medical emergency, hang up and dial 9-1-1. If you are calling about COVID testing…”). Eventually, I stumbled upon the right number to make an appointment. I thought it might be months away, especially given that the clinic is only held weekly. But I got an appointment for February 16th. Hooray! The man on the phone gave me the address and parking information and asked if I had any questions. I asked how long the appointment would be.
“They’re usually about fifteen minutes.”
“Fifteen minutes?” I repeated, shocked. This world-renowned cerebral palsy clinic, where you’re fully evaluated and referred to any number of specialists goes by the same maddenly inadequate fifteen-minute increments as a regular doctor’s appointment? “This is for the adult cerebral palsy clinic?” I clarified.
I was assured that yes, it was, and that was that.
So, we are now making a six- (seven, eight, who knows) hour drive to Santa Monica and staying overnight for a morning doctor’s appointment that might only last fifteen minutes. What, then, am I hoping is the outcome? I am hoping, at the very least, that this doctor will be able to refer me to someone who is experienced in doing labral tear and FAI repair on someone with cerebral palsy. Maybe somewhere closer to us than LA, like UCSF. I’d also like someone to care and understand and listen and not just suggest a new pain medication, but that is asking too much in this culture.
So, I am still struggling, in all areas of my life, as I know so many of us are. I am still making some efforts to stretch and exercise. Occasionally, I even put on my ExoSyms. I had been trying, through November and December, to put them on and practice more regularly like I had been before the labral tear. But when I do, then it hurts more for days afterward. I think I am just not in a place mentally or physically to use them right now. I want to return to them someday soon, but just now, I’m putting what little energy I have into, you know, basic functioning.
I am reading The Book of Joy and using its accompanying gratitude journal. I am trying to meditate regularly, but not succeeding. I’m also looking into calming the vagus nerve, and I think it’s amazing and weird that a nerve can affect so much of the body and mind.
Caring for mental health is always important, and it’s even more vital when physical health feels so precarious. Do what you can to take care of yourselves, everyone. I’ll be here, trying to do the same.