5 October–25 October
On Monday, October 5th, I went back to my primary care doctor to follow up regarding my throat pain. Because my pain is worse, she put an “urgent” note in to the GI, and my referral for January was moved up to October 22nd. How is that possible? Did someone less urgent get bumped? All I have to do is complain more and suddenly there’s a spot for me, not months in the future, but days? So I had a couple of weeks to feel really anxious about being sedated and getting an upper endoscopy. I had not realized this would be the next step, and it feels a little like overkill. My other choices were to go to another ENT, or go the holistic health route. These are all very different levels of treatment–how am I to know the best option?
I have tried to recommit to wearing my ExoSyms and doing my PT at home. A few days, I have done 100 squishes at lunch time in the time it takes for the microwave to heat my food.
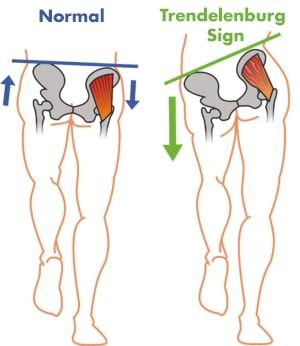
October 8th was the first day with a high in the 70s (78), since…May? And the air quality was moderate. So I went for a walk outside. At 4:30pm. After work. Instead of immediately taking my Exos off. The walk felt pretty good. I’m going faster and I’m less like a wobbly colt. Afterward, my tailbone was achy. I notice that my spastic diplegia aches and pains are more quiet the less I do. Activity wakes them up. It’s an unfortunate truth that right now, I feel better pain-level-wise the less active I am. Despite the mild temperature, I was covered in sweat when I made it back home. And I was glad that I had gone.
Here’s an update from October 9th:
I have continued my daily meditation practice. One meditation I tried begins by telling you to say to yourself, “May I be well. May I be happy. May I be peaceful. May I be loved.” Then you think of someone you love and wish them, “May you be well. May you be happy. May you be peaceful. May you be loved.” You do the same for an acquaintance or someone you don’t know, like a cashier you see regularly, and then the same for someone in your life that you don’t get along with. It was an interesting exercise, but I didn’t quite feel joy flowing out of me like my guide encouraged me to feel.
On Saturday, October 10th, my husband took us on a day trip. On the freeway, a vehicle alongside us had those “my family” stickers on their window. But instead of cute little stick people and a dog, the “family” was different kinds of guns. I felt horrified, disgusted, deeply sad, and deeply mystified how anyone could become whoever that person was. And then I thought, “May you be well. May you be happy. May you be peaceful. May you be loved.” It surprised me, as I struggled against judging that person, that I recalled those wishes from the meditation that had felt foreign and awkward. I don’t believe that the thoughts of peace and happiness I sent out to the person in that car changed them in any way. But they changed me. My feelings shifted from horror and disgust to peacefulness. And that is a good change.
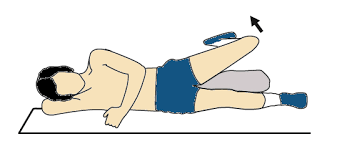
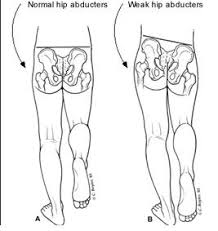
On the 14th, I had my thirteenth PT session with Exos. C did the required strength measurements again and noticed that my glutes are stronger. I could already feel this, so I’m glad it’s noticeable for my therapist as well. We streamlined my home program after I told her how I’d attempted and adapted the clock from last session. Now we are focusing on mat work without Exos, really trying to get my core to engage consistently and build stamina so it actually works when walking. Obviously, weight shifting and walking practice with Exos on is still expected as well. Our plan going forward is to meet every other week rather than weekly.
Here’s what I looked like on October 18th:
And here’s the side-by-side comparison for months three and four:
On Thursday, October 22nd, I had the upper endoscopy. Before and after the procedure were unpleasant, but the thing itself is a complete blank. Thank goodness. Everything looks “normal,” as I figured it would, based on the ENT follow up I’d had. Except for some “granular mucosa” in my esophagus. Maybe that will be something?
I feel like doctor-patient communication has a long way to go. I had never before met this doctor when he came to my curtained cubicle to go over my history prior to the procedure. We’re in a very loud environment, both wearing masks, and I feel like we’re not speaking the same language. Somewhere in the huge litany of questions, I told him I was diagnosed with celiac disease in 2018.
“You have celiac disease?”
“I had the blood test.”
“And who did that?”
“Dr. —”
“Who?”
“Dr. –” I’m referring to the integrative health doctor who ordered a slew of labs for me two years ago, but whom I haven’t seen since because I feel like every doctor should treat the whole patient, and that I don’t want to schlep to Sacramento when I can walk to my local hospital.
“I don’t know that name.”
“I think she even works in this building.”
“Oh, I know who you mean. The gold standard is an endoscopy, so I can take a biopsy while I’m in there.”
“Well, I haven’t eaten gluten in two years.”
“You haven’t eaten gluten in two years?”
“No.”
“Well, I don’t think anything will show up then.”
“Right.”
Many people choose not to (or can’t afford to) follow up a positive celiac blood test with an endoscopy. Did he think I was just going to ignore the blood test and keep eating gluten? I know any damage I may have had will probably have healed by now.
What I would like is for a doctor to review a patient’s history and test results himself instead of quizzing a highly anxious patient in a chaotic environment in which he can’t properly hear. I can’t remember the results of all my labs, nor do I know what they mean.
It’s over now, and I await the results of the biopsies taken. Though rest assured I will ruminate about the whole thing for a while to come. For instance, he asked me about chest pain, and I think I said I didn’t have any because “chest pain” makes me think of heart issues. But actually, the honking cough I have makes my chest hurt quite a bit. Is it burning? I think he asked about that? What did I tell him? And why didn’t he ask about SIBO? SIBO is common with celiac. I wish he had tested for that… How does a throat that hurts this much have no outward signs of inflammation? Do I have some sort of pain feedback loop going on?
Whatever I said to this doctor, he said it didn’t sound like reflux (ENT diagnosis). I tested his theory Friday night by eating chocolate (vegan, gluten free, really good dark stuff). Chocolate is not advised with reflux. Cue a huge uptick in throat and chest pain on Saturday and today.
On Saturday, while I had the house to myself, I did a nice long meditation and then I did my exercises and put on my ExoSyms for a more focused, extended practice session than I’ve had in a long time. In spite of all this non-CP related pain and health crud, I’m still trying to get stronger and use my Exos.