Like many, many adults with cerebral palsy, I learned long ago that “not progressive” means that the damage to the brain does not progress, but cerebral palsy’s effects on the body most definitely DO worsen over time. Because we are told CP is not progressive, and because most healthcare professionals don’t know much about CP, we who are living with it are on a guideless journey of mostly unpleasant discovery. Thankfully, the internet has enabled us to connect with each other. We are each other’s only companions in the dark. Does anyone else…? What do you all do when…? How do you handle…? Of course, each person’s experience with cerebral palsy is different, just like with so many other conditions that are grouped under one gigantic umbrella, so we give each other plenty of contradictory, if well-meaning, advice. By the way, people with CP are taking charge and trying to get healthcare to meet our needs. Check out Cerebral Palsy Grows Up!
Since 2019, I have been on a journey of my own that has often left me feeling in the dark. It’s all been documented here, but I want to bring all the heretofore disparate pieces together now so we can see the big picture. Bear with me and my detailed self-involvement. I want this as a record for myself and might as well put it here, too. (I mean, it is my blog of my life with a disability. What do you expect?)
Here’s a not-so-quick rundown of all the moments I’ve deemed relevant to this particular exercise, timeline-style, kind of:
-Date unrecalled (many years): TMJ (jaw) pain and sharp ear pain.
-June 2008: Neck tension episode so extreme, it caused vomiting. Constant neck and shoulder tension, onset June 2016.
-August 2014: Onset of burning toes, especially when cold or wet. Assumed Raynaud’s. (Turns out it’s not.)
-June 2018: Diagnosed with celiac disease. With positive ANA and high centromere antibody. I’ve had my celiac panel blood test done seven times so far, including the original in 2018, when my tTG result read, “ >250.” Normal is <15. Since then, despite a very strict gluten-free lifestyle, subsequent results have fluctuated between 221 and 81.2. I am happy to say that the 81.2 was from August 2024. The only reason I’m going into this much detail about celiac numbers is that the literature states that when the numbers remain high, look for additional autoimmune diseases.
-May 2019: Ongoing sore throat (months). Faint positive for strep. Took antibiotics, but the pain remained, intermittently. This set off my search. The throat pain didn’t seem connected with anything else.
-October 2019: Ongoing throat pain, now constant. Negative strep; ENT referral.
-December 2019: ENT diagnosed laryngopharyngeal reflux (LPR). Prescribed Protonix for three months. April 2020 follow-up postponed because of the COVID-19 pandemic. Unremarkable esophagram (barium swallow test).
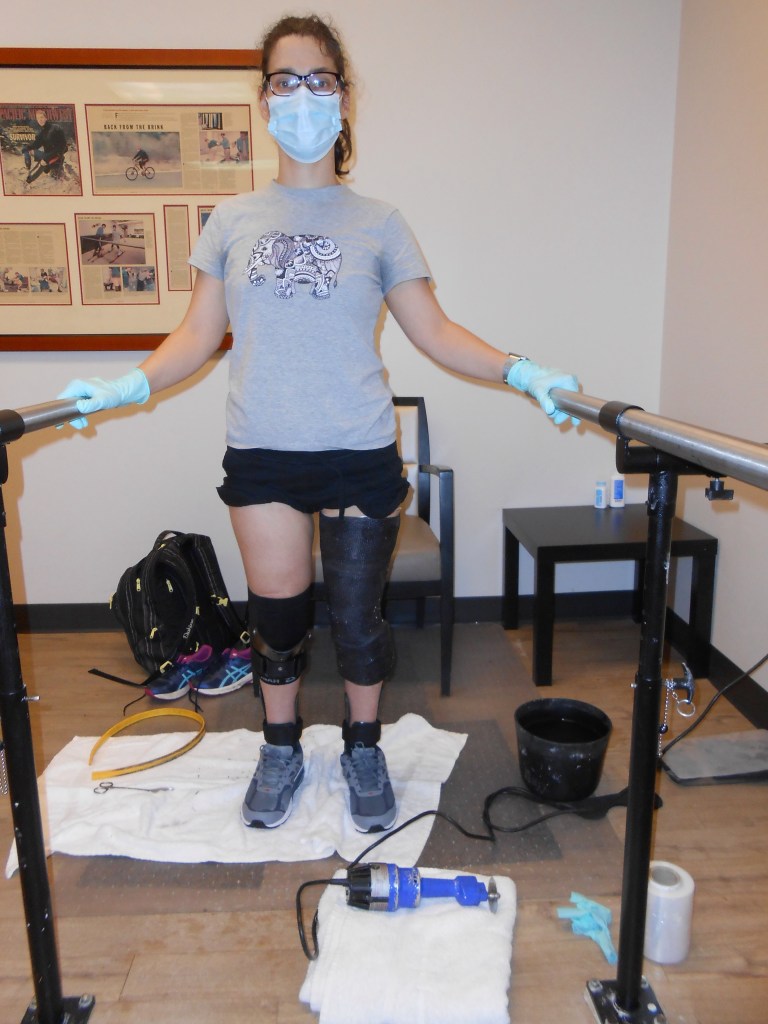
-December 2019: I started using trekking poles to walk longer distances, preparing to use ExoSyms.
-March 2020: Sudden onset of burning forearms, tender/sore thumbs and base of thumb. Loss of grip strength. Suspected cause is trekking poles. Not better with cessation of use. Moderately improved with PT (June–September), but not back to pre-pain function. (This coincided with the pandemic lockdown when everyone’s jobs and lives were upended. I now think that the stress of the sheer number of unprecedented events in 2020 was a big contributing factor.)
-May 2020: H pylori negative. Checked this because of throat pain and reflux diagnosis.
-July 2020: ENT follow-up. Doctor said the inflammation was gone. But the pain was still there. Referred to gastroenterology.
-September 2020: Dramatic increase in throat pain. Chest pain/burning sometimes. Occasional honking cough. GI referral moved up. Avoided acid and caffeine, tried sleeping propped up, no alcohol, etc. Tried Pepto and Mylanta; didn’t help. (This coincided with beginning “distance learning” with my elementary school students. Have you ever tried to teach six six-year-olds how to read via Zoom? This again, I now think, was connected to the unprecedented stressfulness of the world, and the US, in 2020.)
–October 2020: My first upper endoscopy, which was an extremely stressful and emotional experience for me. Results stated “granular mucosa” and “reactive gastropathy with mild chronic inflammation.” No one seemed to think these were concerning or indicative of anything.
-January 2021: GI video visit follow-up. Sent back to ENT (sinuses?).
-January 2021: ENT appointment with a different doctor. Scope showed minor inflammation. Flonase, Claritin, nasal rinse prescribed.
-February 2021: Tried Claritin and Flonase a couple weeks, didn’t seem to help. Same for nasal rinse.
-22 March 2021: Stomach pain and burning woke me up at 5am. Nausea. Throat/reflux felt very strong. Stomach pain eased some with food.
-Spring 2021–Dec 2021: I decided to try seeing a functional medicine doctor. He ordered loads of labs and diagnosed me with Chronic Inflammatory Response Syndrome due to mold exposure. Hard science re: CIRS lacking, but (inactive/prior water damage) mold was confirmed in our home. Mycotoxin urine test showed elevated levels of four mycotoxins, but the test doesn’t have the science to back it up.
-May 2021: Pop in groin. Had MRIs of lumbar and right hip. Diagnosed with labral tear, mixed type FAI, arthritis, probably trochanteric bursitis. Tried steroid injections.
-April 2022: Sports medicine referral at UC Davis: gluteal tendonitis, lumbar facet arthropathy. Sent to PT. Referred for EMG. Tried gabapentin June-October 2022.
-March 2022: Significant increase in beverages/saliva, even food, going down the wrong pipe and causing coughing. Over the past six months? Often daily. Leaves chest hurting.
-April 2022: My PCP had originally suggested ENT or allergist for my throat pain, and we had started with the ENT. So now I asked for a referral to an allergist before deciding whether to tear apart our house to do mold remediation. I had been researching my symptoms, and on RareDiseases.org, I saw something that fit. I asked the allergist about granulomatosis with polyangiitis. He chuckled. (And was right that I didn’t have it).
-May 2022: Forearms still burning. My tTG was back to being very high. Since I also had positive ANA, I wondered if I had an additional autoimmune disease. My new PCP at UC Davis looked at my labs and history and agreed to refer me to rheumatology.
-June 2022: First visit with rheumatologist. No obvious signs of scleroderma, lupus, or other autoimmune diseases.
-June 2022: Leg EMG, nerve conduction study (ordered by sports medicine). Testing for neuropathy: findings “essentially normal.”
-July 2022: Referred to pain management by sports medicine.
-June–November 2022: Tried gabapentin, very low dose to start and worked my way up. First time consistently taking pain meds. Once I was on a standard dose, I stayed on it a while, but I didn’t notice any improvement in pain, and thought I might be starting to experience some side effects, like mild dizziness.
-July–August 2022: Spent two months away from home while brain retraining to see if there was a mold connection. No consistent change in throat pain, but interesting meditation experiences with The Gupta Program.
–July 2022–January 2023: Used The Gupta Program consistently, but no lasting changes.
-September 2022: Pain management doctor discussed compounding cream, CBDa, duloxetine, baclofen pump, and lumbar radiofrequency ablation (but nerves grow back). Referred me to pool therapy, but there are no facilities I can feasibly get to.
-September 2022: Arm EMG (ordered by PCP). “Normal study” with no evidence of peripheral neuropathy.
-September 2022: Right foot and ankle x-ray, at Sutter, for sharp pain that interfered with weight bearing and a new bulge on the side of my foot, onset July 2022. Referred to PT.
-October 2022: First visit with GI at UCD, for “uncontrolled celiac disease.”
-November 2022: MRI for right ankle, at Sutter. Osteoarthritis and not much else.
-January 2023: Tested for strep just in case, before helping a family member post-op. Faint positive again, just as in 2018, but again, no change with antibiotics.
-February 2023: First neurology visit. She was amazed and concerned by my abnormal reflexes and ordered some MRIs. Sigh. Ugh.
-March 2023: Dexa scan (ordered by GI). Low bone density.
-March 2023: Cervical spine MRI (ordered by neurologist). Various mild-to-moderate degenerative changes in places and disc bulges.
-April 4 2023: First appointment with PM&R, at UCD. Fun thing about a teaching hospital is that I had a group of people analyzing and discussing all my various symptoms, and it’s the closest I’ve felt to being in an episode of House, MD. Too bad there weren’t any helpful revelations. “If it hurts, don’t do it.”
-April 11 2023: Brain MRI (ordered by neurologist) because of “abnormal reflexes” in my hands and arms. Only findings: “Small white matter lesion in right brain” that is unlikely to have caused my symptoms.
-May 24 2023: Neuro follow-up. Doctor’s notes include: Small fiber neuropathy could possibly explain her forearm sensory deficit, although she could have mild cervical sensory radiculopathy given her symptoms improved with OT and MRI of C spine did report mild disc bulging at multiple levels. Since her symptom remained stable, symptomatic care for cervical radiculopathy or small fiber neuropathy is recommended, no matter if she does skin biopsy or not. “Symptomatic care” means topical ointment or lidocaine patches.
-June 2023: Endoscopy #2, UCD this time. Very little signs of damage from celiac disease.
-July 2023: I brought up the possibility of fibromyalgia with my UCD PCP. Started Savella in September. Didn’t help. I guess it’s not fibromyalgia.
-September 2023: I was casted at my local Hanger Clinic for a left AFO (recasted and padded in February 2024). Already had one on the right side.
-October 2023: I fractured my right shoulder in a kitchen fall. First panic attack.
-March 2024: I purchased a posterior walker. Started trying it around the neighborhood. Much less labor intensive than using trekking poles, but I’m still not comfortable using it in public (it’s bulky and rattles loudly).
-April 2024: First visit to a new podiatrist. He HELPED my excruciating left big toe!
-May 2024: Appointment with a new neurologist (referred by rheumatologist?) Re: throat and arms. “You have CP.” Referred to otolaryngology and PM&R.
-May 2024: First Teledoc appointment with psychiatrist, because I’m finally open to medication for anxiety. Tried Lexapro. Didn’t seem to help. Tried Prozac next for a few months. Helped but too many side effects.
-June 2024: First Teledoc meeting with counselor. Weird and unhelpful. Had three appointments with her before trying another, who was also weird and unhelpful. Stalled on my quest to find a good therapist.
-October 2024: First visit to UCD otolaryngology for an esophagram and scope. After the scope, he said I have mild laryngeal dystonia/dysphonia. Referred to voice therapy.
-November 2024: PM&R visit #2, with new doctor. No gaggle of students this time. Just a long, detailed one-on-one session, with a few standard strength/tone assessments. Started oral baclofen. Referred to acupuncture.
-December 2024: PM&R follow-up. Increased baclofen. Referred to urology for lifelong, basically, frequency and urgency.
-13 December 2024: First appointment with voice therapist (SLP). He said it doesn’t seem like laryngeal dystonia, but rather just spasticity/increased tone.
There’s a saying in medical school. Well, I’ve never been to medical school, but I heard this way before it was on Grey’s Anatomy, so it must be an established maxim: “When you hear hoofbeats, think horses, not zebras.” In case it isn’t obvious, this saying means that symptoms are most likely caused by a common condition, not an obscure one. You’ve got your overzealous interns coming up with rare diseases, and statistically, it’s more likely to be something that isn’t rare. Horses, not zebras.
Of course, we all secretly think we must be the one zebra in a herd of horses. Just because something is rare doesn’t mean it’s never that thing. It just means that it’s rarely that thing. Someone has to be a zebra sometime. Maybe it’s me. Having access to the internet only encourages our zebra suspicions.
According to my imperfect memory, I grew up without a primary care provider, only seeing physical therapists and an orthopedic surgeon. I never got “sick,” so I didn’t need a doctor. Okay, it’s true that my dad was a GP, so I had a live-in doctor. And he did give me stitches both times I needed them. But my point is, I was, generally, a very “healthy” kid.
I didn’t even know how one went about getting their own primary care doctor, and it felt like a very big step for me in my twenties when I finally did it. I had my own doctor who wasn’t related to me. I had my first pelvic exam. (We in the CP community discuss this adventure regularly. Stirrups are not required!)
I was a kid who almost never needed a doctor, and now I am someone who not only has a primary care doctor and gynecologist but who, in the past six years, has also seen ENT/otolaryngology, an allergist, gastroenterology, rheumatology, sports medicine, pain management, integrative medicine, functional medicine, internal medicine, physical medicine & rehabilitation, podiatry, and neurology. There’s an undeniable element of absurdity in this list. I fully acknowledge that.
I decided to look outside family medicine and seek integrative medicine in my thirties because I was experiencing more and more chronic pain, fatigue, and general decline, and I hoped something more, well, integrative, would help. It was the integrative medicine doctor who tested me, to my surprise, for celiac disease in 2018. If I hadn’t gone to her, I think I would still be undiagnosed. I did not go to her for gastrointestinal issues, but her office took the most thorough history I have ever experienced. Because I do have celiac disease–with panel numbers that have always been out of range, no less–I have a legitimate reason to have a gastroenterologist. Because I have two markers indicating the potential development of other autoimmune disorders (again discovered by integrative medicine), I also see a rheumatologist twice a year (Although these markers were discovered in 2018, I didn’t see a rheumatologist until 2022). It’s still a little weird to me that I have these two specialists that I see regularly now, after being so outwardly healthy my whole life.
The constant throat pain that appeared in 2019 kicked off the ENT/GI journey, and the addition of the burning forearms in 2020 eventually added rheumatology and neurology to my “care team.” Various CP-related issues and injuries led me to sports medicine, pain management, podiatry, and PM&R. Sprinkled throughout were numerous procedures and MRIs that were all the more fraught for being rather inconclusive, except showing that I am, like everyone–but more and earlier–experiencing lots of “degenerative changes.”
It was June of 2022 that I switched over from Sutter Health to UC Davis. When I had chosen my first long-term primary care provider in 2012, I called up Sutter because that was the hospital in town, and I knew how to get there on the bus. I liked my doctor, and after a decade with her, it felt weird to decide to see someone else. Furthermore, because of my childhood associations, I thought of UC Davis as the place you go when you are having surgery, not the place you go for regular healthcare. But I was feeling frustrated and positively worn out, and I wanted to see if I could find answers elsewhere. I didn’t like the idea that one medical establishment could really be better than another, but I decided to find out.
Overall, my experiences at UC Davis really have been more positive than my interactions with doctors at Sutter. The doctors I’ve seen at UC Davis have been more willing to admit when they don’t know something, and therefore also seem more open and friendly, and to genuinely care, for the most part.
I saw a second neurologist in May this year after asking my primary care doctor about vagus nerve stimulation. I have continued trying to find relief for my throat pain–it’s the one thing that still feels unbearable indefinitely. I have tried lots of “acceptance and surrender” with The Gupta Program (which brings together pieces of many different systems, including Buddhism). I do agree with the Gupta Program that “what you resist, persists” (borrowed from Carl Jung). There are plenty of pain studies about meditation and mindfulness. The less you focus on pain, the better you’ll feel. And of course it isn’t easy. There are minutes and hours I don’t think about my throat, and other minutes and hours when I notice my attention on the sensation continually.
After trying Gupta, I kept searching for answers and relief, and I’ve learned a little bit about the vagus nerve. The vagus nerve goes down both sides of the neck, and affects almost every system in the body. There is such a thing as vagus nerve dysfunction, and vagus nerve stimulation (VNS). I thought that maybe I could do 72-hour heart rate monitoring to check my heart rate variability (HRV) and the health of my vagus nerve activity, as suggested by the doctor in this video on the vagus nerve.
However, when you go to a neurologist and ask about vagus nerve stimulation, they are thinking of it in the context of a surgically implant, for treatment of such varied conditions as seizures, depression, and stroke. I was not under any impression that I needed a device implanted in my body. There are many ways of stimulating the vagus nerve that are non-invasive. I just wanted to talk to someone who was knowledgeable about the vagus nerve system as a whole, and how it may or may not be affecting different parts of me.
I have been planning to write about this appointment since it happened in May. By planning, I mean avoiding. So much so, that I had several other appointments that followed it, and I thought, well, I’ll just wait until after this next one and then write about all of it. And here we are on December 31st, and I do not want this task to follow me into the new year (I’ve been writing off and on for weeks). This appointment was hard for me. It was hard because after we talked about my chronic pain and fatigue and increased muscle tone and decrease in function, and also my forearms and my throat, the doctor concluded, “You have CP.” As if this fact explains everything. I sat in the chair and I stuttered, “But, my diagnosis is mild spastic diplegia…” The notes from the appointment state that the doctor suspects “spastic laryngeal muscles.” He referred me to otolaryngology and also back to physical medicine & rehabilitation.
I’ve held on to those words, “mild spastic diplegia,” for my whole life. I heard them as a child while doctors and physical therapists spoke over my head after testing my reflexes and my dorsiflexion and watching me walk up and back, up and back. I’ve read them in my medical records. They are the words I use to explain myself to people and to introduce myself to new doctors. Mild spastic diplegia, affecting my legs.
Over the years I had come to accept that because my spastic diplegia influences my gait and my posture, it will therefore affect my back and shoulders and neck and jaw. However much I didn’t want my CP to affect my upper body, it does. Everything is connected. I was even adjusting to the pain and tension in my forearms being a CP thing. But my throat, too? My throat? No, no, no thank you. If my neverending throat pain is a CP thing, that means I am likely stuck with feeling like I have strep throat for the rest of my life. There, I have written it down now. It only took me about seven months.
Also in May, I had my first appointment with a mental health professional (made months before, not as a result of the neuro visit). I have been wanting to go to therapy for years. I finally decided I was ready to try medication for anxiety, and the psychiatrist I had my virtual appointment with readily diagnosed me with generalized anxiety disorder and prescribed medication. That journey will be a separate post, if I ever get around to it. But it’s been interesting, and has influenced this journey as well. Did you know anxiety meds can cause increased muscle tension? Me either, until I read the long list of possible side effects and then experienced it for myself.
In October, I went to my first otolaryngology appointment. The lovely “barium barista” who guided me through my swallow study told me the doctor I would be seeing was highly regarded. Patients from all over the country came to him when other doctors were at a loss. I talked with the doctor and he put a scope up my nose and down my throat. Then he had me say sentences like, “Please pass the peas and potatoes to papa,” and the other one that is more voiced that I forget, about rain. (That one was harder for me to say.)
He said that it looks like I have mild laryngeal dystonia. Not at the level where he would inject botox into my vocal chords (that’s what he does). I have a diagnosis! Laryngeal dystonia! It is not mold, I am not sick. I just have tight muscles. What was devastating in May almost felt like a relief in October. I think this had a lot to do with the Prozac I was trying at the time, actually. Cue some research as I learned a new word to fold into my identity:
Dr. Judy Gooch
Is it Spasticity, Dystonia or Rigidity
Spasticity and Dystonia: What does it look like?
In November, I saw a new doctor at physical medicine & rehabilitation. She thought trying oral baclofen was a fine idea. Just to recap, the pain management doctor I saw in 2022 was ready to surgically place a baclofen pump, but when I asked about oral baclofen he only said it wasn’t as effective. Two years later, I’m trying oral baclofen. It’s…doing something? On her referral to voice therapy and acupuncture, I saw that she had written laryngeal dysphonia, not dystonia. Cue more research:
Laryngeal Dysphonia from Dystonia Europe
In a talk through Dysphonia International, Dr. H. A. Jinnah said there are terms often used interchangeably: spasmodic dysphonia and laryngeal dystonia: “Laryngeal dystonia is a group of disorders and spasmodic dysphonia is one of them.” The treatment is often botox injections into the vocal cords, but the doctor I saw said mine was too mild for that. While, after seven months of sitting with it, I can wrap my mind around my “mild spastic diplegia” cerebral palsy affecting darn near every muscle group in my body at this point, I still struggle with the expression of spasticity in my throat equaling a constant, strep-throat-like pain. The various manifestations of pain in the rest of my body do not feel like this. And there is something about it being in my throat, my voice, that is less ignorable than in my extremities. My voice feels like me, and for it to hurt all the time, for me to find, not pleasure in singing along with musicals, but pain, has been really hard.
This month I went to my first voice therapy appointment with a speech and language pathologist. He doesn’t have experience with CP, but based on my history of trying all the things and nothing having a lasting effect, he doesn’t think there’s anything he can do. Voice therapy isn’t what I need. It takes muscular strength and breath work to produce sound. He gave the example of a gramophone. The box at the bottom is the muscles, diaphragm, etc. in the torso, and the horn is the muscles in the throat. The vocal cords are just the itty-bitty needle. He’s willing to try massage and muscle taping and teach me (& spouse) to do it ourselves. There are lots of tight muscles in my throat. The pain signal comes from nerves, and there are lots of nerve endings in the throat as well. The baclofen hasn’t decreased my muscle tone enough to reduce the pain of the tension anywhere in my body. I’m back to thinking of round two of The Gupta Program to work on calming my nervous system and its hypersensitivity and constant loop of pain signals.
This year, I also watched the documentary Joan Baez: I am a Noise. I may be completely misremembering this, but I think in an interview segment she watched a clip of herself singing in her early days, and then she was asked straight out if she could still sing like that. She answered, No, I can’t sing like that anymore, and yes, I miss it. Of course, Joan is 83, not 43. I think she didn’t sing publicly for quite a while. Instead, she stayed connected to music by finding joy in dancing. And she painted, because some people get to live lives full of remarkable ability and talent like that. More recently, she has given concerts again. She seems to have reached a truce/peace/acceptance of her voice and her abilities as they are now. It is natural for us to look back and to marvel and wonder at the way things used to be, at what we used to do. For all of us. I can hardly believe I used to walk more than a mile unaided and work for hours straight and then walk some more. (In my twenties. In my thirties I vividly remember the feeling of my pelvis being full of cement and wanting to lie down on the bike path on my way home.)
I think coming to terms with a decline in ability is perhaps easier when you’ve already come to terms with never having had full able-bodiedness in the first place. For me, it’s the pain that’s hardest. And that no matter what, it’s always there. It’s the lack of respite that is exhausting at best and overwhelming at worst. And that is why I’ve spent the last six years searching for an answer to my throat pain. In the hope that one of these things is not like the other. (Throat pain is not like all the other body pain.)
After six years of searching, I finally know that one of these things is like the other. My spastic diplegia isn’t only diplegia. I have to accept that a major part of my identity is no longer what it was. I am not who I was. We continue to be new versions of ourselves, and often we miss parts of the old ones.
I am a horse, not a zebra. I do not have some rare condition with an easy cure. I have cerebral palsy, a very common lifelong disability that affects my muscle tone. Even in my throat.
Now that I sit here on the final day of 2024, after procrastinating and processing for the last seven months, I’m relieved to have finally written it all out. Thank you for reading, if indeed you made it this far!
May we all find moments of peace and happiness in the year to come.